Implementation
The MES moved to a statutory footing on 9 September 2024 – in very simple terms, the MES introduces medical examiner scrutiny to the Medical Certificate of Cause of Death (MCCD) for non-coronial deaths.
The purpose of this guidance is to explain the role and function of the medical examiners, together with the associated practical implications.
Post-implementation feedback from medical examiners
Updated October 2024
Londonwide LMCs had a recent catch-up meeting with our medical examiner (ME) colleagues to find out on how the move of the MES to a statutory footing had gone and these were the key points:
- The uplift in work has meant that this has been a busy time for medical examiner offices, who have been fielding queries from GPs and bereaved families alike.
- The medical examiner offices have in general terms been grateful for the way in which GPs and their practices have adapted to the new procedures.
The following teething issues have arisen:
- Form CN1AThere has been some confusion in relation to circumstances when a coroner issues a form CN1A. In short, a coroner will issue a CN1A to the attending practitioner (AP) when they have decided that their duty to investigate a death is not engaged (in other words when they are satisfied that it has been a natural death). In such circumstances, the coroner will not propose a cause of death and it will be a matter for the AP to complete the MCCD and involve the medical examiner in the (now) usual way.
When a coroner issues a CN1A, they should also inform the medical examiner office to put them on notice of the death but there have been cases when this has not occurred, which has added to the confusion.
In short, if you receive a CN1A then you should complete the MCCD and forward it to the medical examiner office in a timely way (if you have any queries about the completion of the MCCD, then you could speak with the medical examiner and/or the coroner in order to seek their advice).
Further information can be found in Guidance No 47: The Death Certification Reforms – Courts and Tribunals Judiciary.
- Completing the MCCD accurately It makes the system more efficient if the MCCD is completed fully and accurately at the outset (for example – if the ethnicity of the patient is unknown, you should tick unknown on the MCCD rather than leaving it blank).
- Completing the MCCD in a timely way Whilst the vast majority of MCCDs have provided to the medical examiner offices in a timely way, there have been some occasions when there have been significant delays, which has led to additional distress for bereaved families.
It was to be expected that there would be some teething issues as GPs and families become familiar with the new procedures and these should ease wit time.
Please do not hesitate to contact your local medical examiner office if you have any general queries about the new procedures.
Which deaths require notification to the coroner?
The obligation to notify deaths to the coroner can be found in the Notification of Deaths Regulations (2019) (amended March 2020)
If the death does not fulfil the definitions as outlined in the above link, then it will amount to a non-coronial death and therefore will require medical examiner scrutiny (if you are unsure as to whether a death requires referral to the coroner, then the medical examiner will be able to advise you).
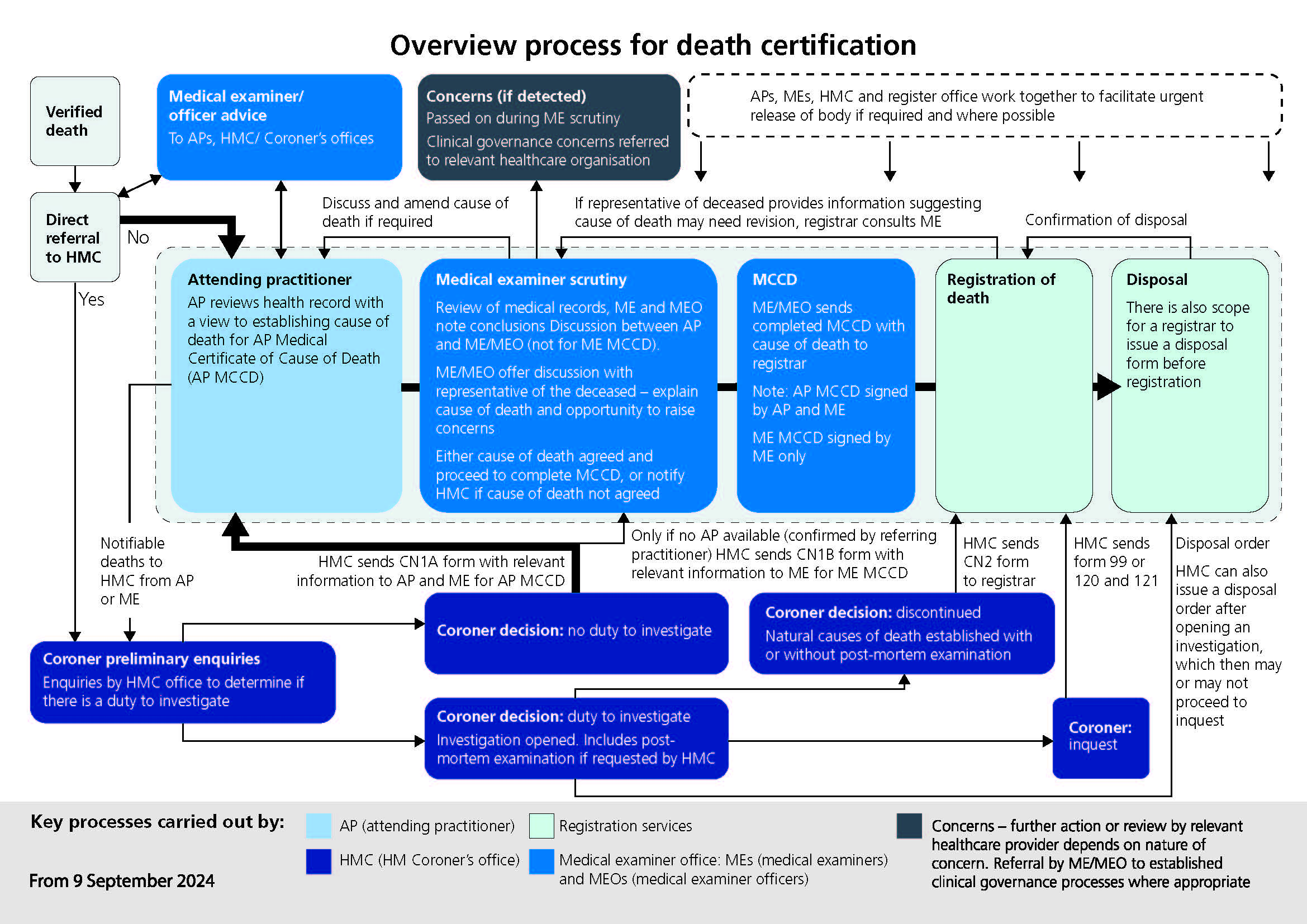
The National Medical Examiner for England and Ways has produced this flowchart explaining the new process.
What is a medical examiner?
Medical examiners are senior medical doctors, who are trained in the legal and clinical elements of death certification processes.
The role of the medical examiner includes:
- Conduct a proportionate review of the medical records.
- Liaising with the doctor who treated the patient in their final illness.
- Agreeing the proposed cause of death with the attending doctor and the overall accuracy of the medical certificate cause of death.
- Discussing the proposed cause of death with the next of kin, ensuring they understand any medical terms and providing an opportunity for them to raise any concerns, comments or compliments that they may have.
- Acting as a medical advice resource for the local coroner.
- Ensuring any concerns about the care of the patient are acted on appropriately (and if possible that any compliments are relayed to the relevant person[s]).
What does a medical examiner do?
Medical Examiners are required to address three key questions:
- What was the cause of death (to ensure the accuracy of the MCCD)?
- Does the death require notification to the coroner?
- Are there any clinical governance concerns (if so a relevant referral should be made)?
The relevant regulations require medical examiners to:
- Provide independent scrutiny of the causes of death in line with their regulatory and statutory obligations.
- Make whatever enquiries appear to be necessary to confirm or establish the cause of death.
- Send completed MCCDs to register offices, once the cause of death has been established.
- Should they detect concerns about care, refer such cases as appropriate to established clinical governance review processes and/or notify the coroner or police when appropriate.
Medical examiners are not responsible for verifying deaths or for confirming the identity of bodies.
Aims of the MES
The stated aims of the MES are summarised below:
- To provide greater safeguards for the public by ensuring proper scrutiny of all non-coronial deaths.
- To ensure the appropriate direction of deaths to the coroner.
- To provide a better service for the bereaved and an opportunity for them to raise any concerns to a doctor not involved in the care of the deceased.
- To improve the quality of death certification.
- To improve the quality of mortality data.
Medical examiner offices
Medical examiner offices in London are hosted by acute trusts.
The table below sets out how medical examiner offices map onto London boroughs.
| Trust/Medical examiner office | London borough(s) |
| Barking, Havering & Redbridge NHS Trust | Barking & Dagenham, Havering and Redbridge |
| Barts Health NHS Trust | City, Newham, Tower Hamlets and Waltham Forest |
| Chelsea And Westminster Hospital NHS Foundation Trust | Kensington & Chelsea and Hounslow |
| Croydon Health Services NHS Trust | Croydon |
| Epsom And St Helier University Hospitals NHS Trust | Sutton |
| Guy’s And St Thomas’ NHS Foundation Trust | Southwark and Lambeth |
| Homerton University Hospital NHS Foundation Trust | Hackney |
| Imperial College Healthcare NHS Trust | Hammersmith & Fulham and Westminster |
| Kingston Hospital NHS Foundation Trust | Kingston and Richmond |
| King’s College Hospital NHS Foundation Trust | Bromley and Bexley |
| Lewisham And Greenwich NHS Trust | Lewisham and Greenwich |
| London North West University Healthcare NHS Trust | Ealing, Brent and Harrow |
| North Middlesex University Hospital NHS Trust | Enfield and Haringey |
| Royal Free London NHS Foundation Trust | Barnet |
| St George’s University Hospitals NHS Foundation Trust | Wandsworth and Merton |
| The Hillingdon Hospitals NHS Foundation Trust | Hillingdon |
| University College London Hospitals NHS Foundation Trust | Camden |
| Whittington Health NHS Trust | Islington |
Contact details for all the Medical Examiner Offices in England a Wales can be found here.
Referral to the medical examiner
In the case of a non-coronial death, the GP who intends to issue the MCCD will need to notify the relevant medical examiner office (this will usually involve completing a brief standardised form and sending it by email to a prescribed email address). Your local Medical Examiner Office will provide details to you on how they wish cases to be referred but this commonly involves completing a brief standardised form and sending it by email to a prescribed email address.
Access to the medical records
Medical examiners have a statutory right of access to the records for the purposes of their role on the basis that they have been added to the list of persons with a right of access to patient records in the Access to Health Records Act (1990).
There is no associated funding to facilitate the provision of the records to the medical examiner. In the fulness of time, this may be resolved by medical examiners having access to the relevant records online, in the interim it is important to work with your local medical examiner office in relation to providing the relevant information that they require.
Issuing the Medical Certificate of Cause of Death (MCCD)
The GP completes the MCCD and if (after scrutiny) the medical examiner is in agreement, then they may simply send an email to the GP confirming that it is appropriate to issue the MCCD.
If the medical examiner does not agree an/or has any queries, then there will need to be a dialogue with the GP in order that agreement can be reached in relation to the proposed cause of death (this dialogue may take place by either email and/or a telephone conversation).
The medical examiner or medical examiner officer will speak with the bereaved family to discuss the proposed entries for the MCCD, ensure they understand the medical terminology being used and give them an opportunity to ask any questions they may have about the proposed cause of death. They will also ask the family if they have any comments on the care provided to their relative, either compliments or concerns they wish to raise.
After the medical examiner scrutiny has been satisfactorily completed (review of the records, speaking with the attending doctor and speaking with the bereaved family member) the Medical Examiner Office will facilitate the disclosure of the MCCD to the Registrar.
There is provision to issue a MCCD (where appropriate) promptly in circumstances when for religious (or other reasons) this is required. However, the same level of scrutiny by the Medical Examiner office is still required to occur for every death.
Legislative changes
The primary legislation that underpins the statutory MES is the Coroners and Justice Act 2009 and since its passage, the act has been amended (most recently by the Health and Care Act 2022) to reflect changes to the health system.
A summary of the changes to the legislation can be found here, however some of the key changes are as follows:
- A medical practitioner will be eligible to be an Attending Qualified Practitioner (AQP) and complete an MCCD, if they have attended the deceased in their lifetime(this removes the obligation to refer the case to a coroner for review if they had not attended the patient within the 28 days prior to death or had not seen in person the patient after death).
- The term attended has not, as yet, been defined however if a GP has made a meaningful contribution to the clinical care of the patient, this is likely to fulfil the definition. Each case will need to be judged on its merits as there may be cases when a GP’s involvement has been minimal or historic. The GP should only complete the MCCD if they feel able to propose the cause of death to the best of their knowledge and belief.
- The new MCCDs (one for the deaths of patients under the age of 28 days and one for patients over the age of 28 days) include the following additional fields:
- The details of the medical examiner who scrutinised the cause of death.
- Ethnicity, as self-declared by the patient on the medical record (if the patient medical record does not include this information, then the attending practitioner can complete it as ‘unknown’ on the MCCD and should not in any circumstance ask for this information from the representative of the deceased).
- Maternal deaths (bringing the MCCD in line with international standards).
- Medical devices and implants will be recorded on the MCCD by the attending practitioner, and this will be transferred to the certificate for burial or cremation (known as the green form) completed by the registrar in order to inform relevant authorities of the presence of any devices or implants.
- The new MCCDs will be in hard copy format, however it will be possible to scan the completed document and forward it electronically. A digital MCCD is currently in development and is likely to be introduced before the end of 2024.
- The scrutiny of the medical examiner’s makes form Cremation 4 confirmation obsolete and the regulatory requirement for the medical referee to scrutinise has been removed.
In practical terms, this means that GPs will no longer be required to complete cremation certification.
Other resources
- RCGP online learning module
- The national medical examiner system (NHS England)
- NHS England medical examiner updates
- Implementing the medical examiner system – good practice guidance
- Medical examiners and general practice (informative video in which two GP medical examiners discuss their experience of the Medical Examiner System to date)
- Guidance for medical practitioners completing MCCDs in England and Wales (new version published to coincide with the implementation of the MES)
Relevant regulations: