From 1 April 2021 vaccinations and immunisations became an essential service and GP practices are required, as part of their GMS contract, to provide vaccinations and immunisations to all eligible patients or target groups within their practice population. A component of the selective immunisation programme is the vaccination of babies born to mothers who have Hepatitis B.
Hepatitis B is known to be more infectious than Hepatitis C or HIV, and those younger people that become infected are more likely to go onto have chronic infection and long-term sequalae, such as cirrhosis and liver cancer. Globally, mother to baby transmission is the most common way to acquire Hepatitis B infection and the programme aims to prevent infants from acquiring the Hepatitis B virus from their mothers by exposure at birth.
Across England 0.4% of pregnant women are found to have Hepatitis B infection (>99% of pregnant women accept screening for Hepatitis B), and the London region has the highest prevalence in the country with 7.07 per 1000 women tested, approximately double the rate of other areas of the country.
The Programme Schedule
Vaccination needs to commence as soon as possible after birth and the first vaccination is normally administered at birth by the hospital within the first 24 hours. There are two more vaccinations required, one at 4 weeks and the other at 12 months, and these are in addition to the normally administered 6:1 vaccination given at 8 weeks, 12 weeks and 16 weeks. It should be noted that the vaccine administered at 4 weeks and 12 months is a monovalent vaccine that needs to be ordered directly from the manufacturer, whereas the hexavalent vaccines which are part of the 8, 12 and 16 weeks programme are normally available. Availability of the specific monovalent vaccine and where to order this vaccine is usually provided in vaccine updates.
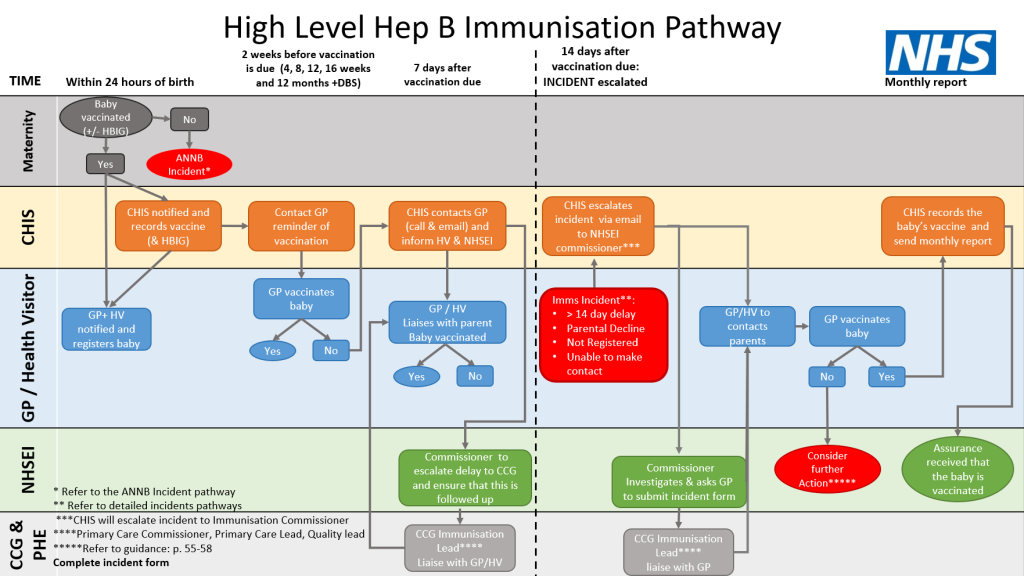
Prompt registration of the infant as soon as possible after birth is the all-important key step that needs to occur, as this will ensure that the baby receives the monovalent hepatitis B vaccination at four weeks, and that the other vaccinations are also correctly timed. London has an enhanced Child Health Information Services (CHIS) in place and CHIS will contact the practice two weeks before the vaccine is due to remind the practice to book the appointment for the infant and order the vaccine.
Practices will need to ensure that staff, clinical or admin, know what to do when they receive communications from maternity services or CHIS, that prompt registration is required and when the additional vaccination appointments need to be booked.
When the infant turns 12 months they will require their final vaccination together with a test for HBsAg (serology or dried blood test (DBS)). When the infant turns 11 months, CHIS will send a reminder to the practice by email asking them to book the appointment for the vaccine and DBS. CHIS will also send a notification to the DBS provider to send out the kit to the practice, clearly labelled with the infants NHS number. The practice will get a result with interpretation, which is to be recorded in the GP notes and sent to CHIS. How to take the DBS sample is described in this video.
The training hub may also be a resource for advice as to how to access any training required.
If the infant is infected, the parents will need to be counselled, and a referral made to a paediatric liver specialist for confirmation and further management.
Classification and management of incidents
If the vaccination is delayed by two weeks or the infant has missed a vaccine, this is then classified as an incident. There may be several reasons as to why there has been failure to vaccinate at the required time, e.g. parent not contactable or the baby has not yet been registered. CHIS escalates this to NHSE/I and the practice then needs to engage with the Health Visitor and the local Health Protection Team if this is felt to be appropriate. The GP practice will be asked to hold a multi-disciplinary meeting to ensure that the baby is vaccinated, and learn from the case and document on the incident form (see attached Hep B Immunisation Pathway).
Summary
The WHO has classified hepatitis as an international public health challenge and in 2016 issued a statement calling for elimination of viral hepatitis as a public health threat by 2030.
In real terms, the actual numbers of babies that will need to be vaccinated is relatively small and this programme provides the opportunity to intervene and prevent the significant consequences to the health of these at risk babies.
For further information, including IoS fee attached to the vaccination:
- BMA reforming arrangements for vaccinations
- PHE (now UKHSA) guidance on the hepatitis B antenatal screening and selective neonatal immunisation pathway
Tell us what you think about our website by completing our quick survey here.

